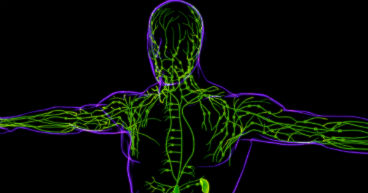
Like a modern building with high-tech features, the human body has a complex infrastructure. The nervous system is like a communication system that sends signals to allow us to think, see, speak and move. The human body also has multiple plumbing systems that carry fluids and other materials through the blood and digestive and lymphatic vessels and out of the body.
When the plumbing gets damaged or clogged, fluid can back up, causing issues that may damage pipes or equipment. That’s what happens when a cancer patient develops lymphedema, one of the most common symptoms and side effects of cancer. With lymphedema, lymph fluid, which carries waste, dead cells and bacteria back into the bloodstream, builds up in areas where the lymph nodes have been damaged, either by cancer treatment or the disease itself. It’s most common in breast cancer patients whose underarm lymph nodes were invaded with cancer cells, damaged by radiation therapy or removed during surgery. Experts estimate that at least 30 percent of breast cancer patients experience lymphedema, although some estimates put that number much higher.
“During a mastectomy, many people may not realize that the surgeon removes a couple of lymph nodes, usually to make sure there are no signs that the cancer is spreading to other parts of the body,” says Ashley Wilson, OTR/L, MS, CLT, Occupational Therapist and Certified Lymphedema and Pelvic Floor Therapist at City of Hope Atlanta. “When that happens, it may cause an impairment of your lymphatic system. And tumors may also impede lymphatic flow, which could cause that swelling or lymphedema.”
According to the American Cancer Society, lymphedema may occur in patients with nearly any type of cancer, but, other than breast cancer, it’s most common in:
- Prostate cancer
- Gynecologic cancers
- Lymphoma
- Melanoma
- Head and neck cancers
Patients diagnosed with lymphedema may have questions about the condition and are likely to go to a search engine for answers. In this article, we’ll answer some of your most frequently asked lymphedema questions on Google, with Wilson’s help. Questions include:
- What causes lymphedema to be more common among cancer patients? Is it the cancer itself or the treatment?
- What are the therapy treatment options for lymphedema?
- Do you recommend compression stockings or compression sleeves for lymphedema?
- How do you help patients manage their compression garments and range of motion issues?
- What’s the biggest mistake patients make with lymphedema bandaging?
- What is complex decongestive therapy?
- Does lymphedema go away?
If you’ve been diagnosed with cancer and are interested in learning about our integrative approach to cancer care, call us or chat online with a member of our team.
What causes lymphedema to be more common among cancer patients?
Cancer may cause lymphedema for several reasons. Among them:
Cancer may spread to the lymph nodes, damaging them and disrupting the normal flow of lymphatic fluid.
Tumors may grow and block or press on nodes or vessels, restricting the flow of lymph.
Cancer treatments, including surgery, radiation therapy and chemotherapy, may also damage the lymphatic system.
“We all have 24 lymph nodes in our underarms,” Wilson says, “So when just two are removed during surgery, that puts extra pressure on the remaining lymph nodes. And sometimes, even more have to be removed. When that happens, the system can become overloaded, so all the excess water, fats, proteins and cells that you normally excrete throughout the day get held in that one area, because the system can’t move it anymore. So, we try to create a different pathway for it to flow through.”
What are the treatment options for lymphedema?
Lymphedema therapy may involve one or more of the treatments below.
Manual lymphatic drainage: Gentle massage is used to move lymphatic fluid from the affected area to healthy lymph nodes.
Compression therapy: Compression sleeves or stockings may help reduce swelling by applying pressure to the affected area.
Exercise: Gentle, low-impact exercises, such as walking or swimming, may help improve lymphatic circulation.
Skin care: It’s important to keep the skin moisturized and clean. “A lot of patients with lymphedema may not realize they're at increased risk for infection,” Wilson says. “So, we try to make sure that they understand that if they get a little nick or cut, it needs to be addressed right away so it doesn't turn into something more aggressive.”
Do you recommend compression stockings or compression sleeves for lymphedema?
Compression sleeves, stockings, bandages or garments are specially fitted over the affected area after swelling has eased. Compression gear is intended to help prevent lymph from reaccumulating in pockets where the fluid had collected.
“There are different levels of compression, depending on your needs and activities,” Wilson says.
Ask your care team about getting fitted for your compression sleeve or stocking to help determine the right type and size of compression device and to better ensure a proper fit. And make sure to learn how to properly take it on and off.
How do you help patients manage their compression garments and reduced range of motion issues?
For many patients, compression sleeves may be uncomfortable and make the limb difficult to move. Lymphedema may make daily activities and routine tasks, such as cooking, cleaning and dressing, more difficult.
“You may not realize how much your body will change or how you're limited when you have lymphedema,” Wilson says. “If your arm is bandaged, it's sometimes a little harder to feed yourself with your dominant hand or brush your teeth or even go to the bathroom. So, we talk to our patients about those types of things and the best ways to work through them.”
What’s the biggest mistake patients make with lymphedema bandaging?
Compression sleeves, stockings and bandages should fit tightly around the affected area, but not so tight that it restricts circulation and blood flow.
“Sometimes, people make their bandages way too tight.” Wilson says. “They come in, and their hands are swelling. That’s because they cut off the circulation.”
Wilson says patients need to wear their compression clothing up to 23 hours a day, removing them only to clean them, bathe and put lotion on.
“You take it off and then put it right back on,” she says. “For a patient with severe lymphedema, that may be a four- or five-week process. That's not something a person might want to do. So, proper bandaging and self-compliance are the two most common mistakes I see.”
What is complex decongestive therapy?
Complex decongestive therapy (CDT) is an umbrella term for an approach to lymphedema treatment that uses the common lymphedema treatments outlined above.
CDT is designed to:
- Reduce swelling
- Increase mobility
- Reduce pain
- Prevent infections and other complications
“It’s everything we do all wrapped up together,” Wilson says.
Does lymphedema go away?
Lymphedema is chronic, and there is no cure. But it can be managed and the symptoms reduced to help patients maintain their quality of life.
“Managing it is the key,” Wilson says. “When you have damaged lymph nodes and you’ve gotten to a stage where you're seeing the swelling, we can manage it to help make sure it doesn't get worse, to reduce your risk of an infection and to try to make sure you don’t continue to get a buildup of fluid in the extremity. And you're probably going to be seen every six months or so to get adjusted.”
If you’ve been diagnosed with cancer and are interested in learning about our integrative approach to cancer care, call us or chat online with a member of our team.