For people with a family history of cancer, genetic testing may uncover critical, even lifesaving clues. If they find out they’ve inherited a DNA mutation that raises their risk for breast cancer, for example, they’ll know to get more frequent mammograms and other screenings, they may be more alert to potential symptoms, they may even opt for prophylactic surgery, as actress Angelina Jolie did. The findings may also affect their family-planning decisions and give their sisters and other family members vital information about their own health risks.
But not everyone qualifies for genetic testing. Inherited cancer syndromes only account for about 5 to 10 percent of all cancer diagnoses, and one in several hundred people have inherited DNA mutations linked to cancer risk. So, people are only recommended for testing if their family history indicates cancer may run in their lineage.
For many, though, the clues are not so obvious. They may not know of other family members who had cancer, or their family history may not show obvious signs of the risk lurking in their DNA, so they may never know of their inherited cancer syndrome, even if they develop cancer.
But that’s beginning to change, thanks to another test that plays a critical role in cancer care: advanced genomic testing, which analyzes the DNA of the tumor itself for known mutations that may be matched with specific treatments, like targeted therapy. Researchers are finding that many cancer patients who didn’t meet the criteria for genetic testing are receiving genomic tests that indicate they may have a hereditary risk of cancer after all.
By their nature, genetic tests are all about assessing risk by searching for inherited DNA mutations, also called germline mutations. On the other hand, genomic tests have long been used to detect acquired (or somatic) mutations, which account for the vast majority of cancers and may have been caused by exposure to carcinogens, radiation, chemicals or other external factors. Now scientists are finding ways to use genomic tests to detect both somatic and germline mutations, and the information is having an important impact, not only in expanding patients’ potential treatment options but in arming their family members with key health information.
“I feel that the ability to predict germline mutations from somatic test results could have a profound impact on any cancer patient, as well as their family’s future journey, if it’s discovered they’re harboring an inherited genetic mutation that was unknown before,” says Vicki Doctor, BSN, OCN, Director of Precision Medicine at Cancer Treatment Centers of America® (CTCA).
Eric Fowler, MS, LCGC, Genetic Counselor and Manager of Clinical Genetics at CTCA Chicago and CTCA Phoenix, remembers working with a lung cancer patient who had genomic testing that discovered a BRCA2 variant, which is often inherited and linked to the risk of breast and other cancers.
“He had no significant family history of any BRCA-related cancers—no breast, no ovarian, no pancreatic or prostate cancer. But just that presence of that marker in the tumor DNA prompted the genetic counseling referral by the oncologist,” Fowler says. “We did genetic testing, and we did find that that BRCA alteration in the tumor was present in healthy cells as well, and therefore was an inherited risk. That was of immense help to his family members, several of whom went on to have genetic testing and tested positive. And we never would have evaluated that person or family or offered genetic testing otherwise.”
DNA key to cancer research
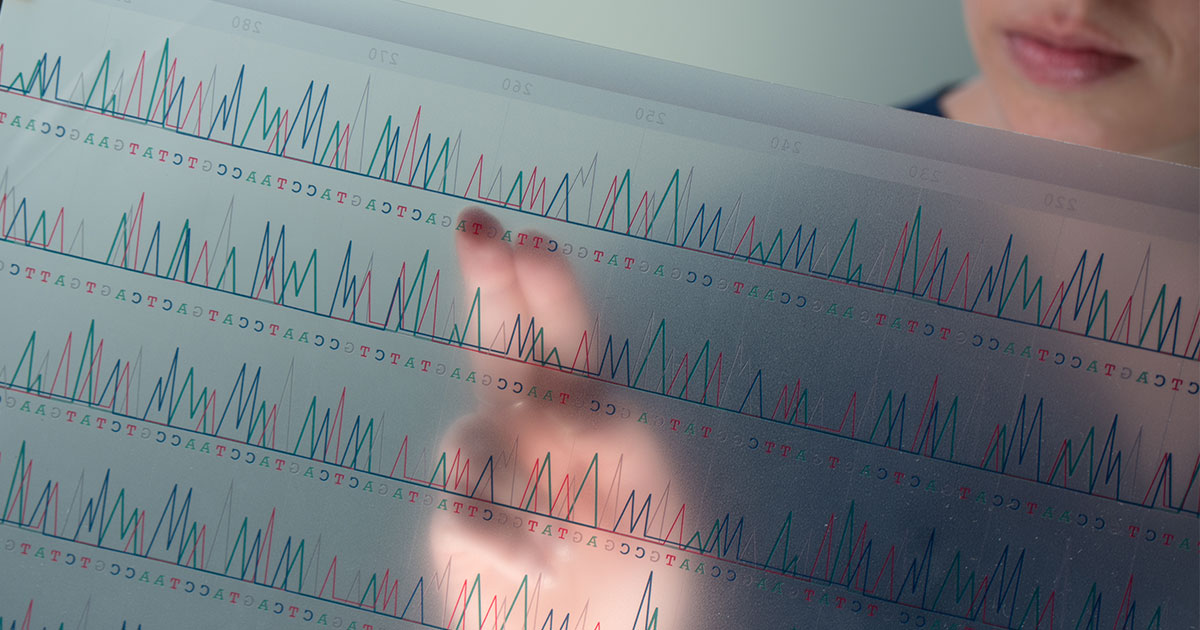
Unlocking the secrets of our DNA continues to provide cancer researchers with new clues for battling the disease by offering a better understanding of the cellular mutations at work in various cancers. A revolution occurred in DNA research in 2003 with the completion of the Human Genome Project, an international effort to sequence the entire human genome. It mapped the human genome’s roughly 3.2 billion base pairs—our genetic “letters”—and its 20,000 or so genes. On National DNA Day, April 25, we celebrate the completion of the Human Genome Project and the anniversary of the discovery of the double-helical structure of the DNA strand by molecular biologists James Watson and Francis Crick.
“This is like a blueprint for everything, from what a person looks like, every trait they have, how their bodies work, even how their cells interact,” Fowler says. “We inherit our DNA from each parent, half from mother and half from father.”
The similar-sounding DNA research fields of genetics and genomics have critical roles when it comes to precision medicine options for treating cancer. Genetics focuses on the hereditary traits passed down from our parents that each of us has stored in the DNA of specific genes in our body, while genomics analyzes the make-up of all our genes—our genome—and how they interact with one another and our environment.
Genetic testing analyzes healthy cells, typically via a blood or saliva sample, and genomic testing focuses on tumor cells. Recent studies have highlighted complementary roles the two forms of testing may have when it comes to identifying potential cancer therapies, especially for patients with advanced cancer or those who have cancers of unknown origin.
Cancerous mutations
The human body has billions of cells that replicate continuously as we age. Cancer forms as DNA mutates, creating abnormal cells that grow unchecked, overcoming the immune system defenses that are supposed to find and destroy them.
The Human Genome Project paved the way for scientists to perform genetic and genomic tests using next-generation sequencing of DNA in either healthy or cancerous cells to identify mutations. One of the goals of testing is to determine whether a patient’s identified mutations match up with some known targeted therapy, creating a sequencing-directed therapy (SDT) option.
The body’s abnormal cells fall into two broad categories:
- Somatic mutations develop or are acquired during a person’s life. They may be caused by non-hereditary factors such as tobacco use, ultraviolet radiation, chemical exposure, viruses and aging. They appear in cancer cells, but not in every cell in the body. Most cancer cases originate from such mutations.
- Germline mutations are inherited, passed from parent to child through the sperm cell or egg during fertilization. These mutations are coded into every cell of the body. More than 50 heritable (or inherited) cancer syndromes have been identified to date.
Genomic tests, because they’re conducted on cancer cells, cannot conclusively determine the presence of an inherited mutation, even though a mutation may resemble a germline variant. A follow-up genetic test is needed to show whether the same mutation is also present in healthy cells, which is the determining factor.
“Just by virtue of the genomic test results, we can’t tell if what we’re seeing is inherited or not,” Fowler says. “To better understand that, a referral to a genetic counselor and then genetic testing will help to differentiate between differences in genes on the genomic test in the tumor that are acquired or are inherited.”
New insights into genomic and genetic testing
What new research seems to show is that inherited risk factors may be more prevalent than previously believed, Doctor says.
An October 2020 study in JAMA Network Open examined the cases of more than 2,000 cancer patients who had genetic testing performed after advanced genomic testing, finding “benefits for further integrating germline genetics into routine oncology testing and patient care.”
“The findings of this study suggest that germline analysis following tumor sequencing often produces findings that may impact patient care by influencing systemic therapy choices, surgical decisions, additional cancer screening, and genetic counseling in families,” the study’s authors said.
In February, JAMA Oncology reported on a University of Michigan study recommending that anyone with advanced cancer receive genetic testing to check for inherited cancer predispositions. It also supports “the use of integrative genomic profiling” as a regular standard of care for patients with cancers of unknown origin and those with other rare malignant neoplasms. “With continued discovery of genomic biomarkers predictive of clinical benefit from anticancer therapies, we anticipate even broader clinical applicability of this technology,” the study’s authors said.
Raising new concerns
More significant use of genetic testing may also create more challenging situations for cancer patients and their families. Someone going in for genomic testing generally is not expecting to be told that an inherited risk factor may be at play. That result may be disturbing to patients dealing with their own diagnosis and who are now being told their family members may also be at risk of cancer.
“Think about, ‘What if I did test positive for a mutation, an inherited risk for cancer? How would knowing that impact me on a day-to-day basis? Is it something that I would be able to put out of my mind until screenings or interventions come up, or would it be something that would be present and thought about more often?’” says Fowler, who provides genetic counseling at CTCA.
Patients should also consider their family relationships “because genetic testing may impact an entire family when an inherited risk for cancer is found,” Fowler says. “For example, if two sisters tested positive for a BRCA mutation but the third sister tested negative, how could that impact relationships among the sisters? Would the sister who did not inherit the mutation have survivor guilt,” even though not having the family mutation was out of her control?
Expanding genetic testing
Genomic test results are increasingly being used as another factor to consider when determining whether genetic testing is warranted. Originally, the guiding factors were more focused just on family and personal histories.
“In general, if a person has been diagnosed with cancer at an earlier than average age, say under 50, or if they have a relative with a diagnosis at an earlier age, that might be a consideration for a genetic consult.” Fowler says. Another factor might be “if you have multiple people in the same family who’ve had the same type of cancer, or even different cancers that may be tracked back to the same inherited risk, such as with Lynch syndrome, where there’s a risk for colon or uterine cancer,” he says.
Other considerations include a generation-to-generation pattern of cancer in a family or a known ancestral connection to cancer, such as among people of Ashkenazi Jewish lineage with family histories of breast, ovarian, prostate and pancreatic cancers.
Fowler sees great potential for genomic and genetic testing in the future.
“I think that there’ll be new genes identified that are linked with inherited risks for cancer, genes that we don’t know about today, cannot test for today,” Fowler says. “I think the genetic testing technologies will be improving, and will be even more accurate than they are today—and they are very, very accurate today. And I think there’s going to be more availability of targeted therapies and treatments—based on finding somebody has an inherited risk for cancer—than we have available today, which are just for certain genes and certain cancer types.”