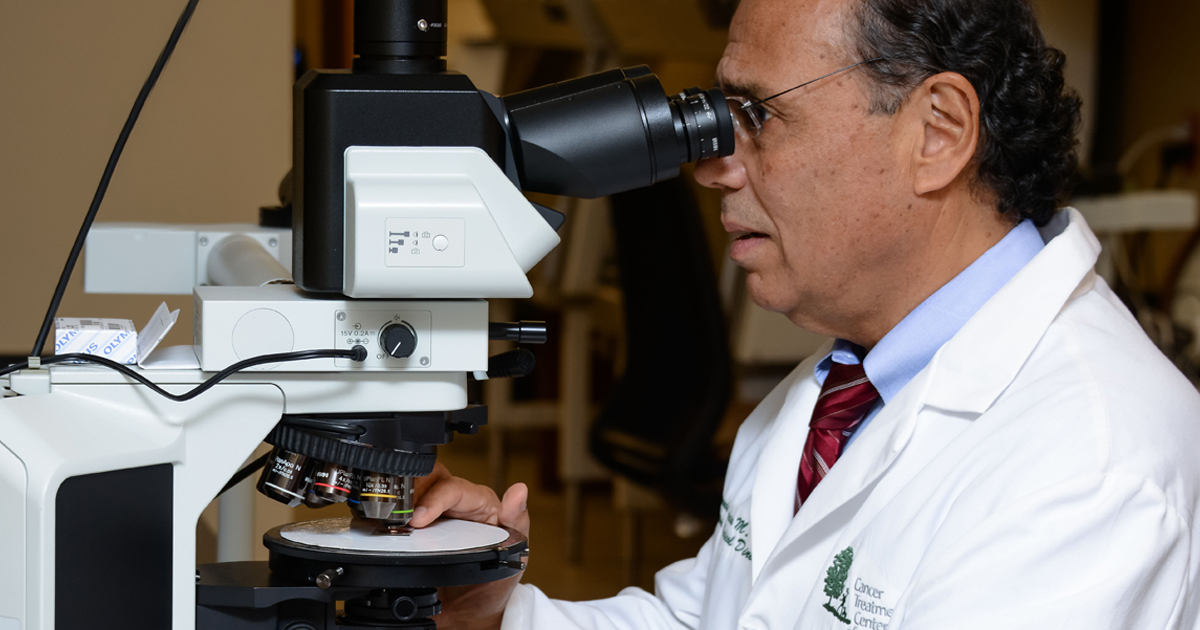
One doctor who plays a critical role in the cancer patient’s journey is seldom seen by patients themselves, but the physician’s mark is felt from diagnosis to treatment. The pathologist is a medical doctor specializing in diagnosing disease by examining organs, tissues, cells and bodily fluids. His or her final product, the pathology report, maps out the cancer’s blueprint, detailing vital data such as the disease’s type, location and stage, all of which help determine the patient’s treatment plan.
“ If you don't have a correct diagnosis, you cannot treat the patient correctly,” - Fernando U. Garcia, MD, Pathologist at our hospital in Philadelphia
How does the process work?
Many standardized procedures are performed before a diagnosis can be rendered. After the patient’s tissue sample is collected during either a biopsy or excision (the surgical removal of tissue), the pathologist conducts what’s known as a gross examination, performed with the naked eye, rather than under a microscope. Observations noted in the gross examination include the sample’s appearance and characteristics, such as size (typically documented in centimeters), texture (whether it is hard or soft, smooth or lumpy) and color. Gross examinations help determine accurate diagnoses because certain tumors have specific characteristics. The distance between the tumor sample’s edges and remaining healthy tissue—called resection margins—is measured and documented. Leaving behind what’s considered healthy margins during the excision is important because it helps the surgeon determine whether all the cancer was removed and whether the patient may benefit from additional treatment.
The sample is then processed in a machine that dehydrates the tissue and replaces it with paraffin wax, which allows the tissue to be cut so thin that light can pass through it. The pieces are placed on slides, which are stained with dyes that change the tissue’s color so they are clearly visible under a microscope. The pathologist then begins a microscopic evaluation. “You must have a baseline for normal tissue,” says Bradford Tan, MD, Chair of the Department of Pathology and Laboratory Medicine at Cancer Treatment Centers of America® (CTCA). “Pathologists understand what normal looks like. We know what to look for and take note of. We look for the presence of a tumor and differentiate what we see compared to what normal tissue looks like.”
The sectioned samples are preserved for future testing, which may be necessary if medical advancements lead to the discovery of a new tumor marker or a new treatment, for example, or if a duplicate slide is needed for the patient to use in seeking a second opinion.
The pathologist needs to identify the type of tumor, which is roughly classified into “five buckets,” according to Dr. Tan. “A tumor that lines a surface, such as the skin or the GI tract, is carcinoma,” he explains. “If the tumor originates from soft tissue like muscle, it’s sarcoma. If it comes from the neural crest (a group of specialized cells found throughout the body), it’s melanoma, and if it’s from blood cells or bone marrow, it’s in the leukemia and lymphoma bucket. The fifth bucket could be a mixture of tumor types or of unknown origin.”
Why is the tumor type important?
Identifying tumor type is key because tumors behave differently. “A treatment for lymphoma won’t work on a carcinoma,” says Dr. Tan. “Sarcoma usually doesn’t metastasize to lymph nodes, but carcinoma often does, and that’s important. One type of cancer requires a lymph node dissection, and another doesn’t.” And some tumor types, such as breast and lung cancers, require additional analysis because they may benefit from targeted therapies. Hormonal markers in breast tumors help identify which drugs may have the greatest impact, for example. “A breast cancer patient with an estrogen receptor-positive tumor typically gets tamoxifen, but a patient whose cancer is HER2-positive would get trastuzumab (Herceptin®), and if none of the slides show hormonal markers, the patient will typically get chemotherapy,” says Dr. Tan.
While all grading systems represent the degree of malignancy, in ascending order, Dr. Tan cautions that grading systems differ by cancer type. “The grading system in one cancer is not equivalent to the grading system in another cancer,” he says. For example, the Gleason grading system, widely used in prostate cancer, is different than the Nottingham grading system used for breast cancer.
Once the pathologist has examined all the tissue samples macroscopically (with the naked eye) and microscopically, and has graded them, he or she stages the cancer, assigning it a number from 0 (zero) to IV, with stage 0 indicating the cancer has not spread from its original location and stage IV indicating advanced disease.
When reading a pathology report, Dr. Tan suggests paying close attention to the tumor type, grade and stage, and he recommends getting a second opinion if you’ve been diagnosed with cancer. “It’s always better to have a second pathologist review the diagnosis,” he says. “You have to make sure that the diagnosis is reviewed and confirmed before you start any treatment. We all trust our physicians. Trust, but verify. Ninety-eight percent of the time, the diagnosis will be correct, but a difference in grading or tumor type could ultimately impact treatment.”